Standard cancer registration
How does the Cancer Registry obtain the cancer diagnoses?
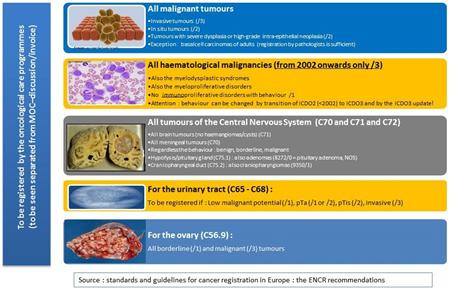
What has to be registered?
Compulsory discussions at the MOC
Under-registration especially when not discussed at the MOC
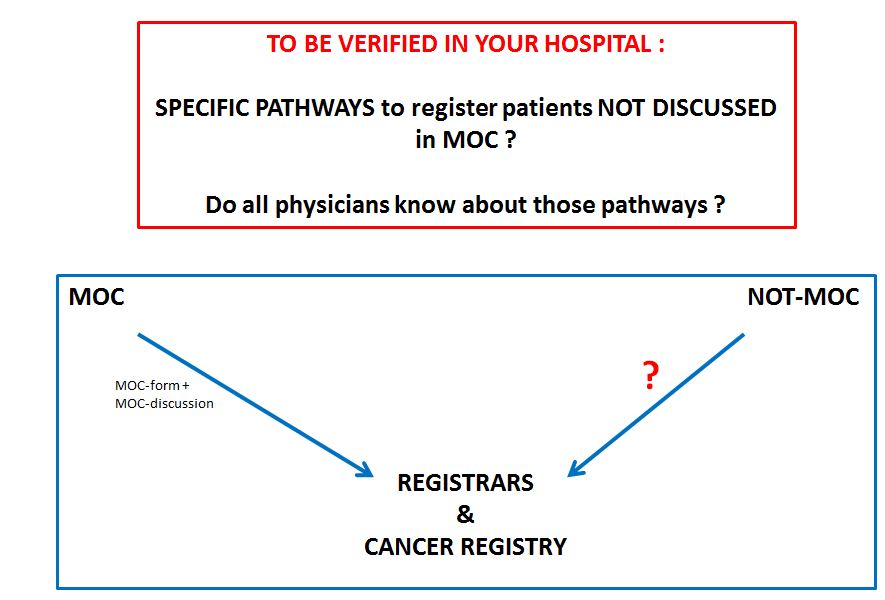
As described in the Health Act of 13 December 2006 and the Royal Decree related to norms for oncological care programmes, all new cancer diagnoses, whether or not discussed at an MOC, must be registered using the standard cancer registration form, as described in the Belgian Official Journal of 14/10/2010.
The standard registration form must be sent to the advising physician, even if the case is not discussed at a MOC.
There are currently two registration forms in circulation: a cancer registration form for a new diagnosis and a cancer registration form for registering follow-up.
Please note: when a new patient is discussed several times at a MOC with regard to the approach of the same newly diagnosed cancer (e.g. before and after surgery), one still uses the cancer registration form for a new diagnosis.
Only when registering a case related to follow-up due to disease progression or a relapse/metastases, the follow-up form should be completed.
Top
How does the Cancer Registry obtain the cancer diagnoses?
- From health insurance funds that send the paper registrations to the Cancer Registry.
- Directly from hospitals:
1. Registration staff complete the standard cancer registration form or the follow-up form using an online application: the WBCR module
2. Using a secured CD-ROM; in this case the hospital respects the requested format
3. Using sFTP, i.e. secured file transfer via the Cancer Registry website. You can find more information in the manual. The green sFTP button in the right-hand column of the screen provides you with easy access to the application. - Directly from anatomical pathologists: who supply the protocols related to the histological cancer diagnoses.
Top
What has to be registered?
Compulsory discussions at the MOC
When the cancer treatment has not been described or deviates from that described in your hospital's oncological handbook.
When use of the chosen chemotherapeuticum is linked to aMOC registration.
When one wants to apply radiotherapy in the same area within a period of twelve months, counted from the start date of the first series of radiotherapy.
Top
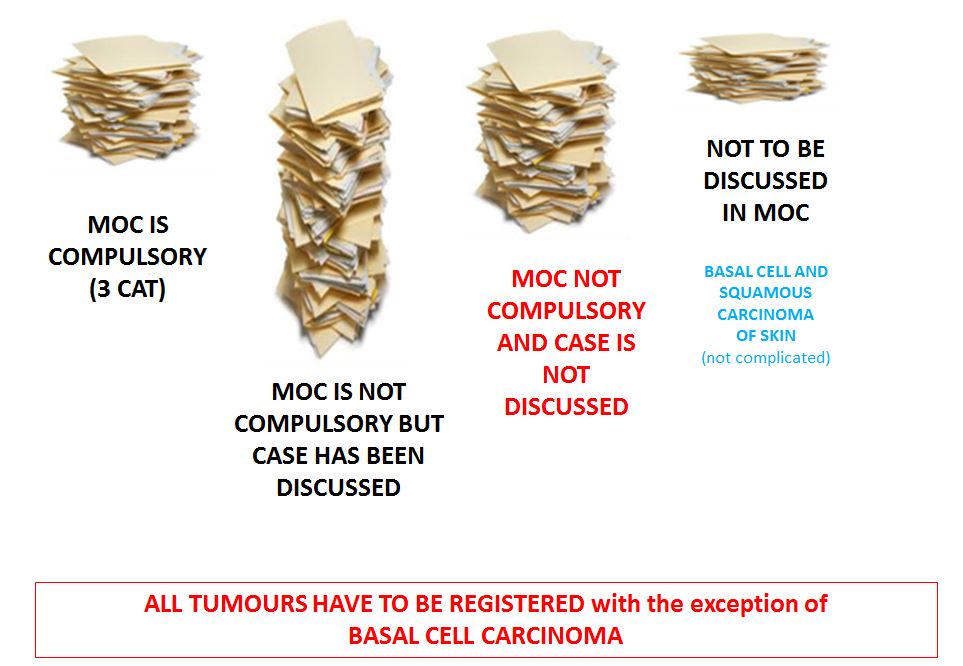
Under-registration especially when not discussed at the MOC
No histological diagnosis
Tumours with difficult biopsy.
Typical examples: tumours in the bile duct, pancreas, lungs and brain, (diagnosis often only by imaging).
Patient dies before histological confirmation could be obtained.
Patient refuses a biopsy.
'Old' cancers that one learns from the patient's medical history and were never registered: important to complete the Cancer Registry's database with regard to later relapses/metastases or follow-up registrations.
The doctor does not wish to discuss it at the MOC
Death shortly after diagnosis
Death soon after starting treatment (e.g. following an oncological intervention)
Diagnosis/treatment refused by the patient
Cancer in which an expectant/palliative attitude is adopted: Prostrate carcinoma, lymphoma, elderly etc.
Cancer whereby the approach is very clear and discussion is not necessary
In accordance with the law no indication for a MOC
Uncomplicated spinocellular tumours (basal cell carcinomas do not have to be registered by the oncological care programmes; supply by the pathologists suffices).
Top